is a minimally invasive surgical procedure that strengthens the cornea to treat and prevent corneal ectasia, such as keratoconus.
Corneal collagen cross-linking (CXL) is primarily utilized to treat keratoconus, a condition characterized by the thinning and weakening of the cornea. This procedure not only helps to stabilize the cornea but also aims to prevent further progression of the disease. Additionally, CXL can be effective for other forms of corneal ectasia, including pellucid marginal degeneration and ectasia that may occur following refractive surgeries like LASIK. By reinforcing the corneal structure, CXL provides a valuable treatment option for individuals facing these challenging conditions.
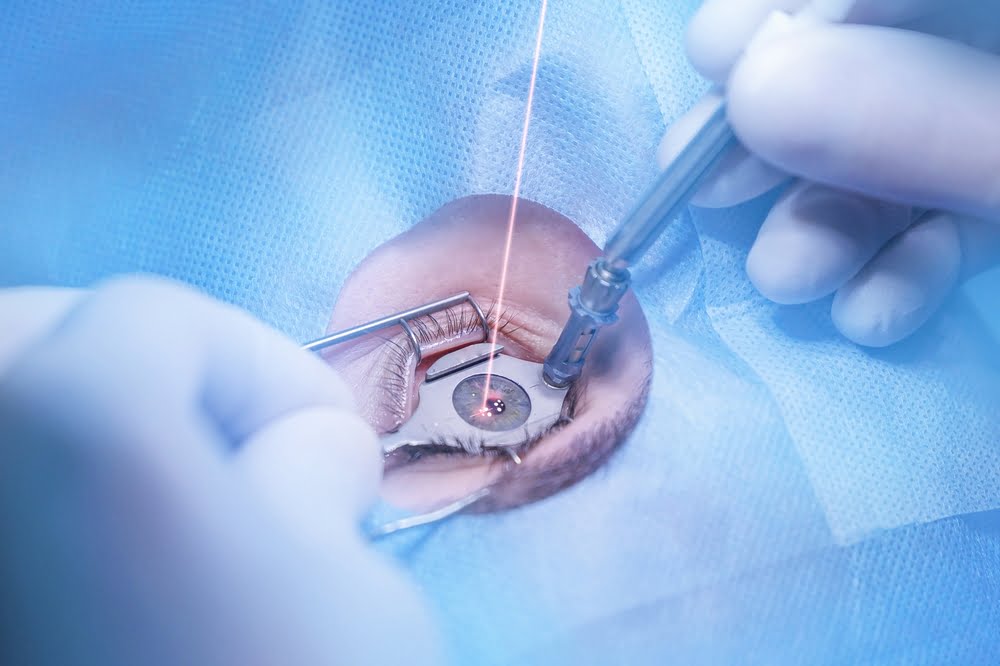
Corneal collagen cross-linking (CXL) is a minimally invasive procedure that strengthens the cornea for individuals with keratoconus and other corneal ectasias. The treatment involves applying a riboflavin solution to the cornea, followed by exposure to ultraviolet (UV) light. This process creates new bonds between collagen fibers, enhancing the cornea's stability. CXL aims to stop the progression of corneal thinning and bulging, helping to preserve vision and improve quality of life.
A photosensitizer is a molecule that absorbs light energy and produces a chemical change in another molecule.
In CXL, Riboflavin is used as the photosensitizer. It is safe systemically and can be adequately absorbed by the corneal stroma topically. It has an absorption peak at 370 nm.
Once exposed to UV-A light, the riboflavin generates Reactive oxygen species, which induce the formation of covalent bonds both between collagen molecules and between collagen molecules and proteoglycans.[5]
Epithelium-off method: As the corneal epithelium offers a barrier to the diffusion of riboflavin to the stroma, the epithelium is manually debrided to enable better penetration. The epithelium-off method is the standard method and remains the most effective.[4]
Epithelium-on method / Trans-epithelial method: debridement induced complications like postoperative pain and corneal haze are avoided with trans-epithelial (epi-on) to avoid epithelium debridement.
These include the use of pharmacological agents to loosen the intraepithelial junctions, the creation of intrastromal pockets for direct introduction of riboflavin, and iontophoresis. Even though debridement induced complications like postoperative pain and corneal haze are avoided, studies thus far have demonstrated lower effectiveness of CXL in this method.[5]
Keratoconus typically begins between the second and fourth decade of life, a time when most people are either completing higher education or establishing their careers. Because the disease is progressive and can be sight-threatening, it often requires ongoing treatments—such as specialized contact lenses or corneal crosslinking—to maintain functional vision, which can be expensive over a lifetime. Consequently, this combination of early onset, progressive nature, and long-term management needs places a substantial economic burden on both patients and their caregivers.”
A Dutch group reported this past year that the number of corneal transplants in the Netherlands was reduced by 25% in the 3 years after the introduction of CXL, compared with the 3 years before its introduction. Nationwide reduction in the number of corneal transplantations for keratoconus following the implementation of cross-linking.
At the recent International CXL Congress in Zurich, Switzerland, Dr. Stulting then reported on 608 eyes, of which only two (0.3%) needed repeat treatment.